Editor’s Note: This post was previously published in Insights on Residency Training, which is hosted by the New England Journal of Medicine and NEJM Journal Watch.
I began one of my PGY2 medical oncology rotations alongside my co-resident: an MD/PhD, fast-track (pre-matched into fellowship) future oncologist. Among my three interns that rotation, two were “Harvard kids.” Needless to say, I was intimidated. My colleague and counterpart not only had the entire catalogue of genomic alterations at the tip of his tongue, he knew and understood their implications on disease. I saw my intern having a long conversation with a nurse at our patient’s door, and when I approached to see if there was anything I could do, I observed him giving a flawless lecture on the approach to an abnormal urinalysis and what really necessitates antibiotic treatment. I wasn’t really sure what I could add to this equation.
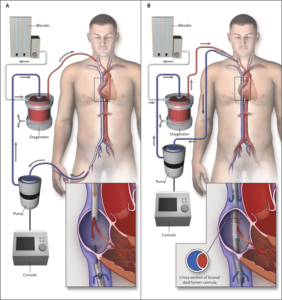
Over the course of the rotation, I found my place, and we all settled in to our roles. We learned from and taught each other different things. We had sick patients, and we took good care of them. When we felt like we’d exhausted all of our medical options to potentially reverse whatever underlying condition that we were attempting to treat, we would joke, “it’s time for ECMO.” When the joke began, I knew what ECMO was, but I didn’t really know how ECMO worked. I silently laughed along, certain that my co-resident and intern possessed superior understanding of this process and would lose all faith in my future contributions to the team should they become aware of my knowledge deficit. But, as we sat at the workstation one day, my co-resident opened Wikipedia and asked, “How does ECMO work exactly?” From there, the intern opened a series of diagrams and images, and we stood together, learning. I look at that experience as an academic “near miss.”
(If you’re curious about ECMO, read this.)
This experience is admittedly mundane, but it highlights one of the turning points in my career. I realized that, for years, I was embarrassed to read. The one piece of advice we’re given as trainees is “read more.” It is tattooed onto our physician-in-training souls. And I did read, but I had been reading “in private,” ashamed to admit that any knowledge deficit existed. I was convinced, each time I read, that I was looking something up that “I should already know.” And yet, there we sat for 5 minutes, looking up something in broad daylight!
 I now know more about ways to learn. Working for 12 or 18 hours and attempting to absorb an article or chapter on the subway ride home is self-sabotage. “Spaced learning” is on the rise. Gone are the days of walking to the library to check out a stack of books. Medicine programs (such as my own), major journals, and academic societies “feed” you information via Twitter. We have infinite access to information in real time and limited time to access it. Despite our own aspirations for perfection, not having infinite knowledge is human. A piece of advice to interns and residents: Ask questions. Look up your own answers. Read more. Let what you don’t know motivate you. Being ashamed to acquire knowledge is a tragedy.
I now know more about ways to learn. Working for 12 or 18 hours and attempting to absorb an article or chapter on the subway ride home is self-sabotage. “Spaced learning” is on the rise. Gone are the days of walking to the library to check out a stack of books. Medicine programs (such as my own), major journals, and academic societies “feed” you information via Twitter. We have infinite access to information in real time and limited time to access it. Despite our own aspirations for perfection, not having infinite knowledge is human. A piece of advice to interns and residents: Ask questions. Look up your own answers. Read more. Let what you don’t know motivate you. Being ashamed to acquire knowledge is a tragedy.
You can read more about the importance of asking questions, what to do when you are new, and how reliance on the internet affects what we think we know on our Learning+ blog:


Like, professor of Internal Medicine/Nephrology, I always recomend, to define first what kind of specialist you want or need to be.After that,one has to develop an complete program(helped by others Physicians or to Read Programs that can have many Medical School)where must be included all the items he/she needs to be reading through the time(He/she, must define the time needed to accomplish his/her goal) After that, it is important to find, books-journals-tplaces and physicians , that can teach to him.
It is important, to include all the skills needed. Besides this,it is important, to evaluate what the candidadte has been learning .One important thing, it is that never forget that the most important technique to learn, it is the Guided Practice, done by specialists and after that, the candidate must do personally all the skills pearned
Could be useful, to use a Gantt card