As opioid prescriptions decline, non-opioid analgesics are increasingly emphasized in a variety of clinical settings as a preferred, safe, and effective first-line therapy for mild to moderate acute and chronic pain.
Examples of Non-Opioid Analgesics
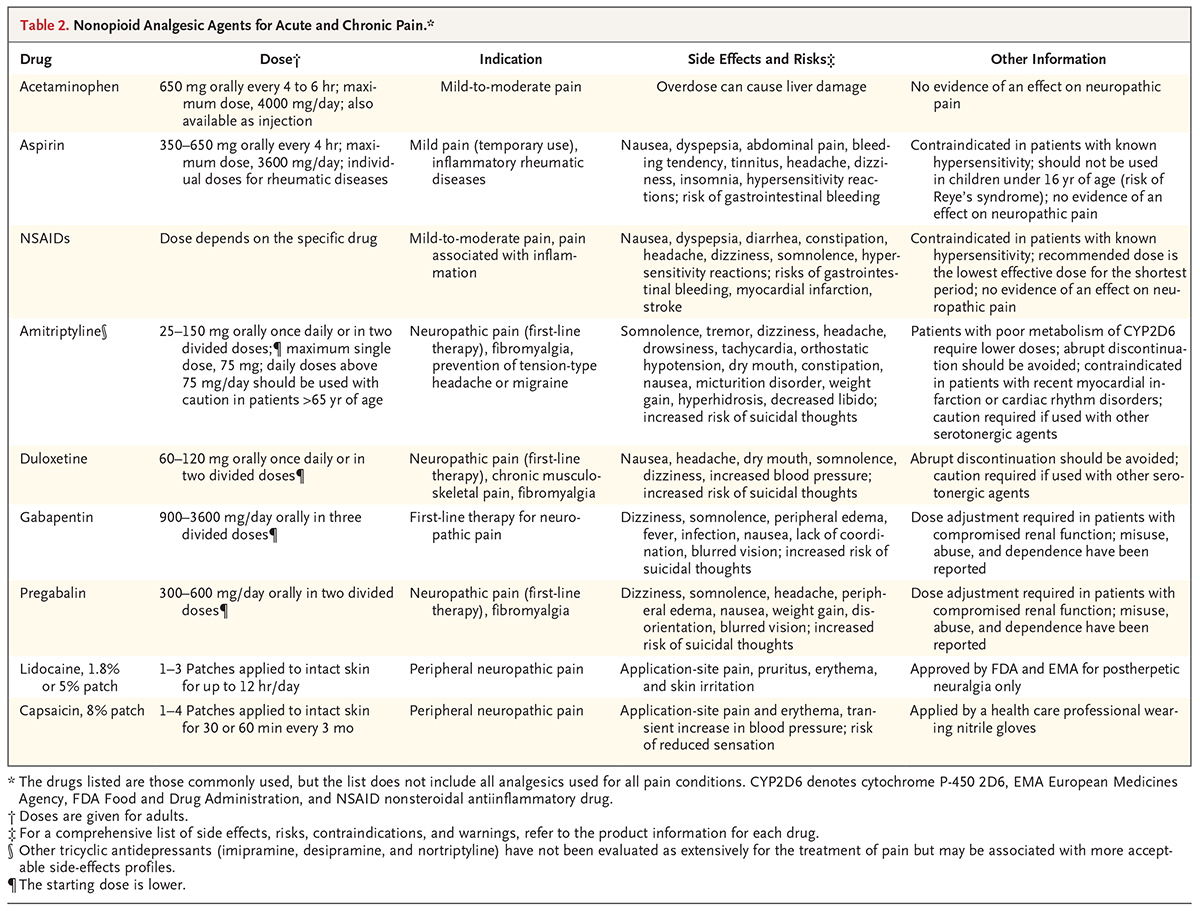
Non-opioid analgesics include a variety of agents, indicated for a number of pain conditions, and carry related potential side effects and risks (see Figure 1). The most commonly used agents include:
- Acetaminophen (paracetamol)
- Anticonvulsants (including gabapentin and pregabalin)
- Antidepressants (including amitriptyline and duloxetine)
- Aspirin (acetylsalicylic acid)
- Other NSAIDs (including ibuprofen, diclofenac, naproxen, and COX-2 inhibitors)
- Topical agents (including lidocaine and capsaicin)
List of Non-Opioid Analgesics
Differences Among Non-Opioid Analgesics
Acetaminophen. The analgesic and fever-reducing effects of acetaminophen are well-known, but its mechanism of action is not. Nevertheless, it is widely considered to be the safest analgesic available, although liver injury is a concern with overdose.
Aspirin and other NSAIDs. Aspirin and other NSAIDs alleviate pain and reduce fever and inflammation by decreasing the synthesis and release of prostaglandins, which are pro-inflammatory molecules. Cyclooxygenase-2 (COX-2) inhibitors also inhibit prostaglandin synthesis and release, but unlike aspirin and non-selective NSAIDs, COX-2 inhibitors do not inhibit platelet aggregation.
Antidepressants. Tricyclic antidepressants (amitriptyline) and serotonin-norepinephrine (noradrenaline) reuptake inhibitors (SNRIs, e.g., duloxetine) have unknown mechanisms for their pain-relieving properties. However, studies suggest that their analgesic effects may be related in part to presynaptic inhibition of the reuptake of serotonin and norepinephrine in pain inhibitory pathways, as well as a peripheral mechanism involving β2-adrenergic receptors.
Anticonvulsants. Anticonvulsive drugs (including gabapentin and pregabalin) provide analgesic properties by lowering neurotransmitter release or reducing neuronal firing.
Topical treatments. Topical non-opioid medications such as lidocaine and capsaicin are applied to the skin and thus act locally. Lidocaine works by blocking nerve signals that send the feeling of pain from the site of injury to the brain. It causes a temporary loss of feeling in the area to which it is applied. Capsaicin appears to deplete local neurons of substance P, which is required in the transmission of nociceptive input.
Are Non-Opioid Analgesics Appropriate for Severe Pain?
The short-term use of low-dose opioids may be necessary to treat the moderate-to-severe acute pain that occurs after surgery or traumatic injury. However, risks associated with opioid use, including the potential for dependence and overdose, have led prescribers to consider non-opioid analgesics — as well as non-pharmacologic alternatives such as cognitive behavioral therapy, exercise therapy, and complementary medicine — to treat mild or moderate acute and chronic pain. CDC guidelines support this practice, noting that nonopioid medications are generally not associated with the development of substance use disorder and recommending “non-opioid medications and nonpharmacologic treatments as the preferred therapies for chronic pain outside of active cancer and palliative or end-of-life care.”
Clinical trials also support this strategy. One study of patients with moderate to severe chronic back pain or hip or knee osteoarthritis pain found that the use of opioid versus non-opioid medication therapy did not result in significantly better pain-related function over 12 months. Moreover, those receiving opioids during the study had significantly more medication-related symptoms over 12 months than those receiving non-opioid analgesics.
Non-Opioid Analgesics in Clinical Settings
Non-opioid analgesics can play an important role in the emergency department and intensive care unit (ICU). For example, a double-blind clinical trial found that for emergency department patients with acute extremity pain, combinations of non-opioid analgesics may be as effective in reducing pain as opioids. And a meta-analysis of 12 randomized clinical trials demonstrated that non-opioid analgesics, used as adjuvants to opioids, reduced the consumption and the side effects of opioids in ICU patients with Guillain-Barré syndrome while decreasing patient pain scores.
Researchers also suggest that non-opioid NSAIDs should become the standard of care for surgical patients to minimize the use of perioperative opioids and to decrease postoperative opioid-related adverse effects such as nausea, vomiting, sedation, ileus, pruritus, and respiratory depression. This finding aligns with the enhanced recovery after surgery pathway (ERAS) strategy, which calls for multimodal pain management. The study’s authors state, “multimodal analgesia is based on the premise that the concurrent use of primarily non-opioid analgesics has additive, if not synergistic, effects that produce superior analgesia while decreasing opioid use and opioid-related side effects.” However, they also encouraged clinicians to seek continuing medical education on multimodal analgesia drug-drug interactions and adverse effects to limit unanticipated consequences of the practice.
Pain Treatment Strategies
Today’s clinicians have a variety of pharmacological and non-pharmacological options for treating pain. For some patients with acute severe pain, a short course of opioids aids in healing and recovery. For other patients with chronic severe pain, opioids provide relief and allow patients to function in their daily lives.
As the medical community increases its focus on safer, more judicious opioid prescribing and reducing the misuse of opioids, health care providers are carefully evaluating all available alternatives — from opioids and non-opioid analgesics to mind-body therapies — weighing their potential benefits against their risks. As new studies and trials of non-opioid analgesics are undertaken, clinicians will have additional evidence for their effective use.
Learn more about how to assess, treat and monitor patients with pain with the NEJM Knowledge+ Pain Management and Opioids free online CME module.
This blog post, originally published on December 19, 2019, was updated on September 14, 2022.

Thank you for sharing information about Pain. My mom is suffering from joint pain, and now she started ayurvedic knee oil. It is effective and gives relief in pain.
Thank you for sharing such a good information about Pain management. It helps me a lot. I tried Topical non-opioid medications. Again thank you.
A great informative article regarding pain management, we should not avoid any type of pain that can lead to serious health problems in the future.
I suffer from severe chronic pain in my torn SI joint, compressed vertebrae, numerous lumbosacral herniated and torn lumbar discs. I have had three carpal tunnel surgeries which have become symptomatic again. On top of all this I am experiencing the arthritic and beginning of frozen shoulders which I continue to utilize regardless of them getting “stuck” and a lot of pain.
Long story longer, I had four hip replacement/ revision surgeries in 2016-2017, thanks to being infected with MRSA during my first surgery. I experienced kidney failure along with multiple allergic reactions to the antibiotics. I was opiate resistant within the first month and was prescribed 800 mg Duexis q6hr. One of the times I was released for a couple days, I saw a wonderful pain Specialist who gave me epidurals and even injected my SI Joint. That is the only way I made it through 2017.
Now, after another kidney infection, my kidney specialist told me no more Duexis/Ibuprofen. So, I am on Gabapentin for nerve pain but that is it. Of course he mentioned Tylenol. What a joke! Tylenol is not even an antiinflamatory! It is like taking a sugar pill when one is in extreme pain! I wish doctors would stop recommending that!
I am seeing my pain Specialist in two days; resorting to epidurals once more. I am anxious to hear the recommendation from my pain doctor in two days.
There are many more people like me who live with blinding pain for life. I only hope someone is looking for drugs, not opiates, to give people like me other options going forward. I am 57 and hate to think I am destined to have injections, hoping they continue to work, for the rest of my life.