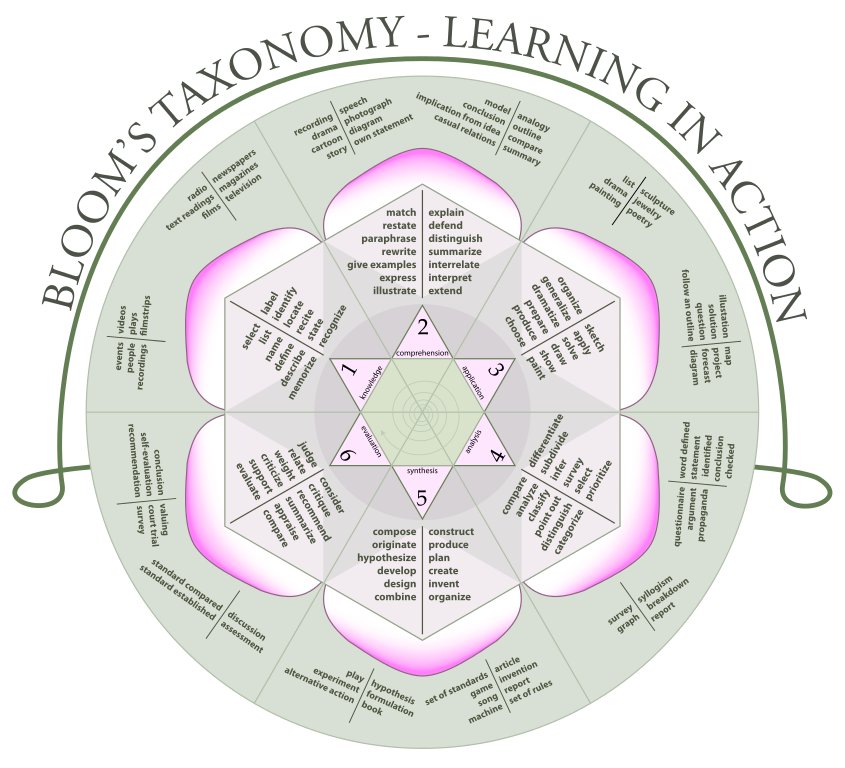
Identify. Recognize. Interpret. Distinguish. What do these words have in common? They are all “Bloom’s verbs” — the foundational building blocks of learning objectives, according to one of the most widely used pedagogic models, Bloom’s taxonomy.
Bloom’s taxonomy is the backbone of most CME and residency programs’ lesson plans, assessments, simulations, and learning platforms—including NEJM Knowledge+.
The actions associated with each level of Bloom’s learning hierarchy — remembering, understanding, applying, analyzing, synthesizing/evaluating, and creating — reflect both educational goals and clinical experience. These actions are a spectrum of simple to complex levels of education: straight memorization of facts all the way up to making judgments about the validity of ideas and an ability to generate new knowledge.
Medical educators need to understand where their learners are on the ladder and tailor their assessments to the learning objectives they write. Students and lifelong learners can improve their recall on exams and in practice by metacognitively defining their goals with Bloom’s-backed learning objectives and self-assessments that show them their knowledge strengths and weaknesses.
How Bloom’s Educational Framework Is Used in Medical Education
Bloom’s taxonomy is an ideal educational framework as it reminds us that the basis of all clinical decision making is knowledge. Students and residents (as well as physicians in practice, one could argue) cannot diagnose and treat patients without a foundation of recalling correct information and comprehension of that knowledge. Applying that material to patient care is the next step up on the ladder: “formulate” a solution to a problem, “map” out a plan for treatment, “prepare” a patient for the next step in evaluation.
It’s also helpful for students of any age to examine their own areas of weakness and strength along the Bloom’s hierarchy. One might be missing some essential facts (such as the clinical features of heart failure) at the bottom level of the pyramid; lacking those facts, it might not be possible to evaluate next steps (such as choosing the most appropriate management approach for a patient with systolic heart failure).
Dr. Roy Phitayakorn is a general and endocrine surgeon and the Director of Surgical Education Research at Massachusetts General Hospital and an assistant professor of surgery at Harvard Medical School. He is also the education R&D consultant to NEJM Group. He says, “I also like to use Bloom’s taxonomy as a framework to formulate my question asking and/or teaching scripts for each level of clinical reasoning. Bloom’s forces me to move beyond simple recall of information and challenge my learners to move up the taxonomy.”
How We Use Bloom’s Taxonomy in NEJM Knowledge+ Learning Objectives
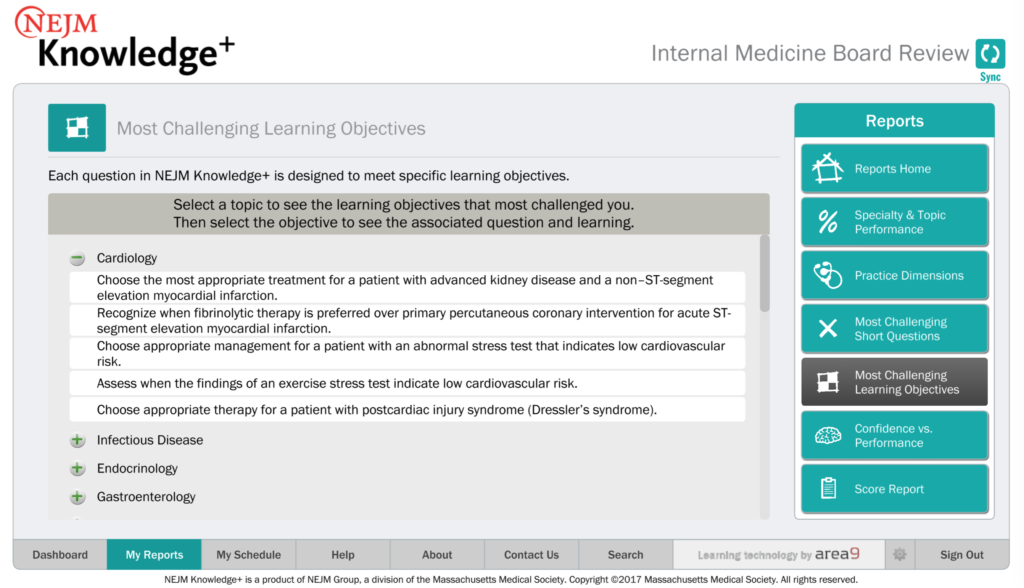
NEJM Knowledge+ uses Bloom’s verbs in all our learning objectives — and they form the basis of all our multiple-choice and fill-in-the-blank questions as well as the detailed explanation we provide with every question, answer, and key learning point.
Our process begins with the writing and editing of learning objectives by our subject-matter experts.
Experts in each field start with their high-level blueprint then drill down into topic-specific learning objectives. Many of our case-based questions assess your knowledge of two levels of learning: the first is framed as recognizing or determining the diagnosis of the patient described in the case, and the second is likely to require you to know how to best manage the treatment or evaluation of the patient. Case vignettes are written with relevance to practice in mind; many of our questions include laboratory findings in a table and images, such as electrocardiograms, CT scans, radiographs, and photographs of skin findings. Our short questions will sometimes summarize these cases (requiring the same two-step reasoning) or skip to providing the diagnosis in the question stem — asking you to choose the best next step, thus assessing only the secondary learning objective. Our fill-in-the-blank questions test you on a single learning objective, but it could be either the primary or the secondary LO.
Learners in NEJM Knowledge+ can see the questions’ underlying learning objectives in the report “Most Challenging Learning Objectives,” which shows the items you have struggled with and allows you to link through to the questions that test those LOs.
Define Your Goals with Bloom’s Verbs
The benefits of defining your educational goals with Bloom’s taxonomy are to put them in a clearly defined hierarchical list. Bloom’s model assumes that you want to master basic knowledge of facts first, then you will be able to move up the pyramid from there — and eventually synthesize the science that’s been proven and to even create new knowledge.
If you notice that many of your wrong answers are because you lack “recall” — a Bloom’s verb at the knowledge level, the base of the pyramid, then you should spend more time testing yourself on the facts.
As you master those learning objectives dealing with remembering, you will move up to the next level: understanding. In medicine, whether you are learning the material for the first time or are a longtime practitioner reminding yourself of information you have forgotten over time, higher-order decision-making skills are often based on a full comprehension of the underlying mechanisms, prevalence, and risk factors of disease.
The focused but detailed feedback section included with every question in NEJM Knowledge+ explains why the right answer is right and all four of the wrong answers are plausible but wrong. We also point to further reading on the topic, often to landmark studies and guidelines.
Research has shown that testing yourself on your knowledge using the spaced repetition model is the best way to improve — both on exams and in practice.
Can You Flip the Bloom’s Pyramid?
Bloom’s model of education assumes, as I have discussed above, a stepwise accrual of knowledge and skills, beginning with memory of facts and progressing to comprehending, applying, analyzing, synthesizing, and evaluating/creating. But what if you tried to flip the pyramid?
The flipped classroom exercises the idea of students using valuable class time not for sitting passively while listening to the teacher talk but for exploring ideas in groups, with projects and access to the teacher during the activities. Learners absorb information in lectures, slides, videos, and texts at home, before they attempt the in-class assignments. Ultimately, this model does not really flip the Bloom’s pyramid, because it assumes that students are learning the facts, understanding them, and only then applying, analyzing, and synthesizing in class.
Could You Begin by Evaluating or Creating?
Some argue that a true flipped classroom is one where students actively use their minds to test theories, encounter a concept before grasping all of its history, and grapple with discovery — the opposite of building knowledge on the basis of rote memorization. Being actively involved in generating new conclusions is meaningful and may help motivate students.
In the world of medicine, the real test of your knowledge is when patients’ lives are at stake. Would flipping Bloom’s model work to teach clinicians what they really need to know to diagnose, evaluate, and treat patients in the real world?



Humble thanks! Doctor Josh
Recognizing the good presentation and the idea that Medical education must follow Benjamin Bloom Taxonomy, I only would like to add, that Bloom´s say that there are 3 levels of knowing=
1)Information=Ex= when you know something reading an newspaper or seeing TV , but you are not sure that those events really happen.Or you Know, that Paris, is the capital City of France, but you never have been there.
2)To know by sight(in Spanish=conocer):=that means that you have been in Paris only as Tourist.Or, in Medicine=you have seen only an Appendicectomy, buy you never did one.
3)To Know=(in Spanish=saber)= you really are aware of some knowledge or skill , because you did it before.Or, you lived in Paris, for a long time.Obviously, the final goal in Medicine is to dominate some Speciality or Techniques.we use in our lives the · levels described by Benjamin Bloom